Mothers of children with autism have different metabolite levels
Blood sample analysis could help predict risk of disorder
Above: Research by ASU President's Professor James Adams and Juergen Hahn of Rensselaer Polytechnic Institute indicates blood sample analysis could help predict whether potential mothers are at a higher risk of having a child with autism spectrum disorder. Photograph courtesy of Pixabay
Blood sample analysis shows that, two to five years after giving birth, mothers of children with autism spectrum disorder, or ASD, have several significantly different metabolite levels compared to mothers of typically developing children.
A multidisciplinary team from Arizona State University, Rensselaer Polytechnic Institute and the Mayo Clinic analyzed blood samples from 30 mothers whose children, between the ages of 2 and 5 years, had been diagnosed with ASD as well as 29 mothers of typically developing children. The research has been published recently in BMC Pediatrics.
The team found differences in several metabolite levels between the two groups of mothers. When examined further, researchers were able to group those differences into five subgroups of correlated metabolites.
While the samples analyzed were taken several years after pregnancy, these research findings raise the question of whether the differences in metabolites may have been present during pregnancy as well.

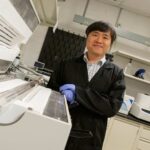
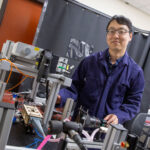
President’s Professor James Adams
“Based on these results, we are now conducting a new study of stored blood samples collected during pregnancy, to determine if those metabolites are also different,” says James Adams, a President’s Professor in the Ira A. Fulton Schools of Engineering and director of the Autism/Asperger’s Research Program at ASU.
Adams and co-author Juergen Hahn, the head of the department of biomedical engineering at Rensselaer found that many of the variances were linked to low levels of folate, vitamin B12, and carnitine-conjugated molecules. Carnitine can be produced by the body and can come from meat sources like pork or beef, but there wasn’t a correlation between mothers who ate more meat and mothers who had higher levels of carnitine.
According to Hahn, this finding suggests that the differences may be related to how carnitine is metabolized in some mothers’ bodies.
“We had multiple metabolites that were associated with the carnitine metabolism,” Hahn says. “This suggests that carnitine in mothers is something that should be looked at.”
The team’s big data approach proved to be highly accurate in using a blood sample analysis to predict which group a mother belonged to, and this suggests that the development of a blood test to screen for mothers who are at a higher risk of having a child with ASD may be possible.
“A blood test would not be able to tell if your child has autism or not, but it could tell if you’re at a higher risk,” Hahn says. “And the classification of higher risk, in this case, can actually be significant.”
This research builds upon Hahn’s and Adams’ other work. Hahn previously discovered patterns with certain metabolites in the blood of children with autism that can be used to successfully predict diagnosis. He has used this same method to investigate a mother’s risk for having a child with ASD. He and Adams have also done similar work in children with autism who have chronic gastrointestinal issues.
By combining Hahn’s expertise with Adams’ extensive research into biomedical issues associated with ASD, including nutritional deficiencies and microbiome abnormalities, this work exemplifies the interdisciplinary model for education and research at Rensselaer and ASU.
Written by: Torie Wells, senior communications specialist, Rensselaer Polytechnic Institute