Brain injury research explores sex-dependent therapeutics
Above: Arizona State University Associate Professor Sarah Stabenfeldt and University of Texas Health Science Center at Houston Associate Professor Rachael Sirianni are leading the first exploration of sex-targeted drug delivery for traumatic brain injury in a five-year, $2.5 million project funded by the National Institutes of Health. The project will improve the fundamental understandings of sex differences in traumatic brain injury and help design more effective nanoparticle delivery treatments. Graphic by Erika Gronek/ASU and Shutterstock
Nearly two million people experience a traumatic brain injury in the United States every year. Just as each person is different, their injuries present in different ways.
This complexity means people who suffer traumatic brain injuries may not receive effective treatments that heal the core injury to the brain. But one factor — how the injuries differently affect females and males — brings unique challenges and opportunities for future treatments.
Sarah Stabenfeldt, an associate professor of biomedical engineering in the Ira A. Fulton Schools of Engineering at Arizona State University, and Rachael Sirianni, an associate professor in the Vivian L. Smith Department of Neurosurgery at the University of Texas Health Science Center at Houston, are leading the first exploration of sex-targeted drug delivery for traumatic brain injury.
The five-year, $2.5-million project funded by the National Institutes of Health will improve the understandings of sex differences in traumatic brain injury to help design nanoparticle delivery systems for more effective treatments.
“A concussion or head injury can cause lasting impact,” Stabenfeldt says. “Prevention can minimize that, but we also need to do better about diagnostics and therapeutics. There’s so much we don’t know or understand.”

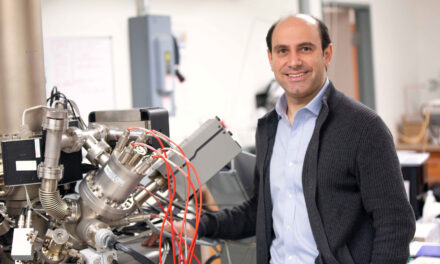
Sarah Stabenfeldt, an associate professor of biomedical engineering in the Ira A. Fulton Schools of Engineering at ASU, is a co-principal investigator on a National Institutes of Health-funded research project to understand sex-dependent brain injury response and explore sex-targeted, nanoparticle-based treatments. This photo was taken before the current pandemic social distancing and face covering requirements went into effect. Photographer: Marco-Alexis Chaira/ASU
Understanding traumatic brain injuries
Depending on the severity of a brain injury, many different outcomes can occur. Symptoms range from bleeding to inflammation and other disruptions to normal functions, and they can change over the hours and days following the initial injury.
Our brains also appear to display sex-dependent biological differences relevant to injury and treatment.
“When you look into the clinical literature, it has been shown that males and females do report differential symptoms, and females report more prolonged symptoms after a head injury,” Stabenfeldt says.
A key sex-dependent discovery about traumatic brain injuries is the disruption of the blood-brain barrier.
In their normal state, blood vessels in the brain are very restrictive about what they allow into the brain. They protect it from substances that might hurt neuron cells — creating a very carefully controlled blood-brain barrier. In other parts of the body, however, blood vessels allow all sorts of nutrients, waste and other substances to transfer between vessels and cells. After a traumatic injury, the brain’s carefully controlled system falls apart.
This disruption also presents differently in females than in males. One of the many factors that could be causing this difference is varying levels and cycles of sex hormones such as estrogen, progesterone and testosterone in females compared to males. While these levels already differ in healthy people, brain injuries also cause additional hormone disruption for both sexes.
The complexity is daunting, but it’s also why Stabenfeldt says she is really excited about this research and its potential to improve traumatic brain injury outcomes. Such an opportunity led her and Sirianni to propose a grant to the NIH.
“If we discover that this differential blood-brain barrier disruption is a function of sex hormones, it gives us a clue about whether those hormonal processes should be targeted,” Sirianni says. “The information from this work could tell us whether that’s important in designing therapies in the future.”
Their team is the first to look at injury-impaired hormone systems when assessing their role in treatment.
“If we’re basing our dosing on healthy models, but the pathology completely changes how the body is going to respond to, uptake and process different pharmacological strategies, then we’re going to be really off base when we’re trying to develop therapeutics,” Stabenfeldt says.
Building on an exciting discovery
Stabenfeldt and Sirianni’s project expands upon research conducted by a former doctoral student from Stabenfeldt’s research group who was co-advised by Vikram Kodibagkar, associate professor of biomedical engineering at ASU.
Vimala Bharadwaj, now a postdoctoral scholar in the Department of Anesthesiology, Perioperative and Pain Medicine at Stanford University, focused her doctoral research at ASU on investigating the breakdown of the blood-brain barrier after a traumatic brain injury in animal models and how it can be used as a unique delivery window for nanoparticle-based treatments.
It was a difficult line of research in which Bharadwaj had to navigate many failures, but she was motivated by working in such an exciting area of research. She came out the other side with notable successes that have far-reaching implications. It was Bharadwaj’s observations that led the team to hypothesize that brain injuries may present differently across sexes.
“Specifically, we demonstrated that the nanoparticles accumulate near the injured brain tissue via the disruption of the blood-brain barrier,” Bharadwaj says. “Next, we discovered that the blood-brain barrier disruption and consequent nanoparticle delivery was sex-dependent, where the females showed prolonged and extended blood-brain barrier disruption compared to males.”
This laid the critical foundation for researchers to understand sex-dependent differences in the pathology of brain injuries.
Stabenfeldt didn’t expect to see these results, and when she shared them with Sirianni, she was very excited.
“When you see something so fundamentally biologically different, it means there’s an opportunity to utilize that biology in some fashion,” says Sirianni, who was not involved in the research with Bharadwaj. “We are also therapeutically oriented and want to ask, ‘Can we utilize that difference for a therapeutic end goal to benefit the way we treat traumatic brain injury in males versus females?’”

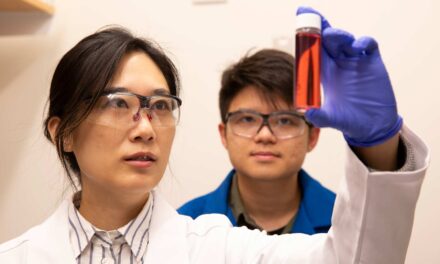
Sarah Stabenfeldt (left) and Vimala Bharadwaj (right) discuss research in the Stabenfeldt Lab in 2015. Research Bharadwaj led as a doctoral student laid the foundation for understanding and potentially harnessing sex differences in traumatic brain injury expression and treatment. This photo was taken before the current pandemic social distancing and face covering requirements went into effect. Photographer: Jessica Hochreiter/ASU
A new treatment strategy
In addition to the possibilities of exploiting blood-brain barrier disruption differences in males and females, nanoparticle systems also provide researchers a new avenue to evaluate drug treatments.
Systemic drug delivery through an IV or pill means dosages have to be safe for other organs and systems in the body. Drugs administered in these ways also get filtered out of the blood quickly, and repeated doses have a rollercoaster effect of cycling high and low concentrations of the drug reaching the injury.
Drugs that were previously seen as unsafe or ineffective when given systemically can instead be targeted directly to the injury microenvironment through nanoparticle delivery systems.
“With these nanoparticle systems, we’re looking at how we can revisit a drug that showed promise in preclinical studies or clinical trials but then failed,” Stabenfeldt says.
Stabenfeldt and Sirianni are assessing a strategy in which they exploit the disruption of the blood-brain barrier to have their nanoparticle-based treatment accumulate in the injured region of the brain for a longer, sustained local delivery.
Nanoparticle-based therapeutic delivery systems also show strong sex-dependent differences, so the team will explore how to most effectively use them in female and male injury microenvironments.
This work is also an important step into more inclusive research that involves females as well as males, who until recently have been the scientific standard. When preparing for the NIH grant, Sirianni said she found very little existing research that explored nanoparticle interaction in female versus male biological systems.
“I’m excited that we’re going to be contributing to some of that knowledge,” Sirianni says. “We really want to impact both the basic understanding of why there is differential pathology and also achieve a therapeutic, translational goal of identifying sex-specific therapies. If we can identify ways that nanotechnology could target male versus female pathology, that would be truly transformative.”
Multidisciplinary team collaborates for complex research
Research into such complex systems would not be possible without a multidisciplinary team collaborating to achieve a common goal.
Targeting nanoparticle delivery to unique sex hormone microenvironments in an injury environment takes many different areas of expertise and experience working with complex human and drug delivery systems.
“Every time you bring diverse ideas and diverse approaches into a room, it’s going to improve the kind of science you can do,” Sirianni says. “The way we interpret and understand the data will absolutely benefit from more individuals being part of it. This particular topic intersects many fields, so by necessity, it’s essential to have many contributors.”
Christopher Plaisier, an assistant professor of biomedical engineering in the School of Biological and Health Systems Engineering, one of the six Fulton Schools in which Stabenfeldt also teaches, brings expertise in systems biology and informatics to help the team determine the role of complicated factors such as hormone cycles and regulation.
Outside of biomedical engineering, Heather Bimonte-Nelson, a professor of psychology in the ASU College of Liberal Arts and Sciences, lends expertise in how sex hormones change in animal and human systems. Jason Newbern, an associate professor of genomics, evolution and bioinformatics in the ASU School of Life Sciences, will contribute to the project’s behavioral studies. And Trent Anderson, an associate professor of basic medical sciences at the University of Arizona College of Medicine, will assist with visualizing nanoparticle distribution.
Sirianni has a long history at ASU, from earning her bachelor’s degree in bioengineering to working as an ASU adjunct professor while maintaining a primary faculty appointment at Barrow Neurological Institute.
Sirianni says prior work with Stabenfeldt, Bimonte-Nelson and exceptional ASU graduate students on other multi-disciplinary projects has opened the door to fruitful collaborations between labs and universities and garnered interest from federal funding organizations.
“When you develop these collaborative teams and working relationships, knowing how you can benefit one another and integrate skill sets and expertise is a really important part of doing impactful work,” Sirianni says.
Research reported in this publication was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under Award Number R01NS116657. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.