Battling addictions with engineering algorithms
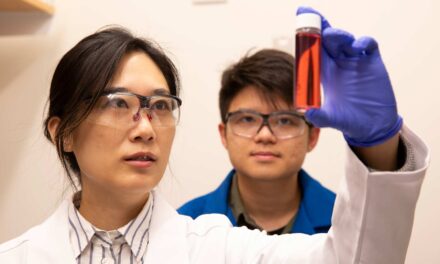
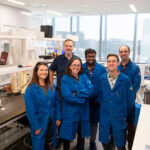
Daniel Rivera (center) is applying concepts from control engineering to behavioral health treatments involving addiction intervention. His research team includes biological design doctoral student Kevin Timms (left) and chemical engineering doctoral student Yuwen (Shirley) Dong. Photo by Jessica Slater/ASU
Posted: May 17, 2011
Chemical engineers are responsible for numerous scientific advances, ranging from affordable pharmaceuticals and super-strong synthetic fibers to environmental cleanup and recycling technologies. Most people don’t associate engineers with advances in behavioral health, but new research shows engineers might have much to offer those fighting addictions and other behavioral disorders.
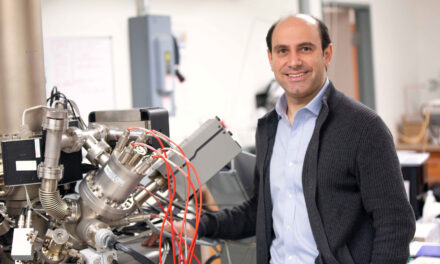
One of the leaders in this unlikely collaboration is Daniel Rivera, a professor of chemical engineering in the School for Engineering of Matter, Transport and Energy, one of Arizona State University’s Ira A. Fulton Schools of Engineering. Rivera is also program director for ASU’s Control Systems Engineering Laboratory. He and other engineering researchers are applying concepts from control systems engineering to behavioral health interventions.
“Experts in behavioral health have already realized that not only is it necessary to provide treatment over time, it has to be adapted to participant response. We’re using ideas from engineering to optimize how to deliver adaptive interventions,” Rivera says.
Control systems engineering is the field that develops algorithms to automatically adjust variables in a system based on measured responses. Everyday examples of control systems include the home thermostat, cruise control in a car or an insulin pump. There are even natural control systems within the human body.
Since control systems automatically adjust variables based on measured outcomes, they are an ideal technology for adaptive behavioral interventions, which must change dosages as patients progress in their treatment. In this case, a dosage could refer to the amount of medicine a patient takes or the type and frequency of counseling they receive.
In a 2007 study published in the journal Drug and Alcohol Dependence, Rivera used a hypothetical intervention to demonstrate how control systems engineering could be applied to help address a behavioral health concern.
The proposed intervention aimed to improve parental function in families over the course of three years. Research shows that poor parental function is linked to conduct disorders in children and adolescents, including drug and alcohol use.
The intervention is expressed as a feedback control system in which the frequency of family counseling visits changes over time, based on a quarterly assessment of parental function. The intervention also accounts for potential disturbances in the family, such as job stress or depression.
This approach relies on something called a “dynamical systems model” to make optimal dosage decisions over time. In previous behavioral health interventions, researchers have used simple “if-then” rules that are not as personalized, resulting in less successful outcomes, Rivera says.
Engineering and behavioral health researchers believe that the control systems approach of tailoring treatments based on participant response could improve behavioral health treatments. Conduct disorder is just one topic within the field of behavioral health, which also includes the complicated issue of addiction.
Rivera co-wrote a 2011 review published in the inaugural issue of the journal Translational Behavioral Medicine that examines how adaptive interventions for smoking, weight loss, disease management and treatment adherence can be implemented through mobile devices, such as smart phones. The issues chosen for the study are all considered chronic relapsing disorders, which require continued care over an extended period of time.
In order for these interventions to be effective, participants must report updated information about their experience with the treatment on a regular basis. Few people have time to meet with a health practitioner every day, but 85 percent of American adults have cell phones, according to the Pew Research Center. This could be a convenient way for behavioral health patients to receive computer-tailored feedback and support during their treatments.
“Individuals participating in a smoking cessation intervention could be prompted through their iPhone or similar device. The information received from a patient is used by a feedback control algorithm to make a decision and provide a treatment recommendation.” Rivera says. This method ensures that patients are receiving advice specific to their current needs.
Jack Chisum, a behavioral health specialist and professor in ASU’s College of Nursing and Health Innovation, says that changing a behavior such as smoking or eating unhealthy foods is very difficult for patients, who often feel the habit is a part of their identity.
Chisum has also found many patients worry that if they succeed in quitting, they will have to limit the time they spend with friends or family members who still smoke or use.
“We don’t have a really good history of people starting programs and staying with them. They start, stop, start and stop. It may be part of human nature, we don’t know,” Chisum says.
However, behavioral health experts have found that intervention programs tailored to each individual patient are twice as successful as programs that do not offer individualized treatment.
Another way to increase patient success is to identify an effective support mechanism.
“The patient might come see me three times a week for an hour. My influence on them may be strong at that time, but it may not surpass all the temptations they have throughout the day,” Chisum says, which is why continuous support is so critical for behavioral health patients.
Since most people carry their cell phones with them at all times, text messages are a logical delivery method to provide patients with support. Additionally, applying concepts of control systems engineering to the text message interventions could personalize them even further and allow for more precise adaption.
Combining engineering principles with behavioral health interventions is a non-traditional approach, but one that has significant potential. The Office of Behavioral and Social Science Research and the National Institute on Drug Abuse, centers within The National Institutes of Health, have awarded Rivera $1.4 million to do this research. Rivera says that despite how different the two fields are, he saw promise in the collaboration.
“That’s part of working in transdisciplinary research,” he says. “It becomes imperative to establish connections between fields.”
Written by Allie Nicodemo
Note: The other authors of the 2011 Translational Behavioral Medicinestudy are: William T. Riley, National Heart, Lung, and Blood Institute, NIH; Audie A. Atienza, National Institute of Health, National Cancer Institute; Wendy Nilsen, Office of Behavioral and Social Science Research, NIH; Susannah M. Allison, National Institute of Mental Health, NIH; and Robin Mermelstein, University of Illinois at Chicago.