Frakes’ research team helps advance virtual artificial heart implantation

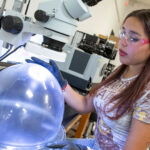
ASU engineer David Frakes and biomedical engineering doctoral student Justin Ryan discuss a 3-D heart reconstruction, designed using software developed by Materialise. Photographer: Jessica Hochreiter/ASU
Some firsts in the history of artificial heart implantation are being achieved by an Arizona State University research group and medical professionals at Phoenix Children’s Hospital.
They have performed what they believe is the first virtual implantation of a pioneering artificial heart, and an implantation of that artificial heart in an undersized adolescent patient.
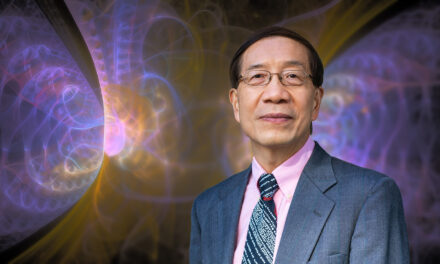
The ASU team is led by David Frakes, an assistant professor in the School of Biological and Health Systems Engineering and the School of Electrical, Computer and Energy Engineering, two of ASU’s Ira A. Fulton Schools of Engineering.
Frakes has been working with technology developed by the Tucson-based company SynCardia Systems Inc., which has developed the Total Artificial Heart for adult patients with end-stage biventricular heart failure who are waiting for a permanent heart transplant.
Frakes is using advanced software developed by the Belgium-based company Materialise to generate 3-D reconstructions of cardiovascular, respiratory and skeletal structures that provide a virtual screening of pediatric patients that helps ensure a proper fit of the artificial heart in the patients.
Through that technique, Frakes aided a Phoenix Children’s Hospital team to map procedures for the first-ever virtual implantation of the Total Artificial Heart. The actual device was implanted into a 14-year-old boy, one of the smallest pediatric patients to date to receive a Total Artificial Heart as a bridge until actual heart transplantation can be performed.

Frakes examines a 3-D print of an optimized, patient-specific artificial heart that was virtually implanted into a pediatric patient. Photographer: Jessica Hochreiter/ASU.
He says that initially the Total Artificial Heart was implanted into the teen, but complications arose. Images were obtained at the hospital and an accurate 3-D model was made by engineers at ASU. The 3-D data set helped reveal the reason for the complication, allowing the team to create virtual implantations for small patients who will need the Total Artificial Heart in the future.
A virtual implantation is used to assess the fitness of pediatric patients for an actual implantation of the Total Artificial Heart, particularly those whose body stature could complicate implantation, such as pediatric patients or patients with skeletal abnormalities.
“This cutting-edge technology helps medical interventionists and surgeons plan complex procedures,” explained physician Stephen Pophal, chief of cardiology at Phoenix Children’s Hospital. “With the help of the bioengineers at ASU, we can see if devices designed for adults can fit in children. This is especially important as a newer and smaller version of the Total Artificial Heart is awaiting Food and Drug Administration approval and promises to benefit many children with severe heart disease.”
Frakes’ team performed the virtual implantation of the heart in the patient using Materialise’s Mimics Innovation Suite’s diagnostic technology to create a 3-D reconstruction of the adolescent’s chest cavity from a computerized tomography (CT) scan, and then used a laser scan of the Total Artificial Heart to virtually place the heart into the chest cavity.
After the implantation, a clinical review and a series of measurements – called a virtual fit analysis – determined whether the Total Artificial Heart could properly fit into the boy’s chest cavity. Phoenix Children’s Hospital has adopted this procedure for use with all future Total Artificial Heart candidates.
The artificial heart supported the boy for 11 days before he underwent a heart transplant.
“It literally helps pump blood through a patient’s body because their own heart can’t,” says Frakes, explaining that the Total Artificial Heart isn’t a long-term solution, but it keeps patients stable until a heart for transplant is available.
“It can also increase quality of life during the waiting time,” says Justin Ryan, a doctoral student on Frakes’ research team. In many cases, patients are able to freely move around during the wait time with the use of a transportable external driver component connected to a small mobile battery pack.
The virtual implantation technology isn’t only a significant achievement for care of pediatric patients, Frakes says.
“Virtual implantations can help bridge the gap between heart failure and transplant in congenital patients of all ages,” he says. “They can help optimize a proper fit during pre-operative planning so that complications are minimized by orienting the device in the chest cavity correctly.”
Frakes says his team and partners at Phoenix Children’s Hospital plan to continue the use of virtual implants pre-operatively to identify suitable candidates for the Total Artificial Heart and other cardiac-support devices.
“Many patients may be labeled too small for the device, based on standard criteria, when their body may actually accept it,” he says. Virtual implants and fit analyses will help to show compatibility on a case-by-case basis.
SynCardia has a smaller Total Artificial Heart in development that is designed for patients of smaller stature. But with the current model, implantation into such patients could be risky without the pre-operative virtual implant.
Frakes documented Phoenix Children Hospital’s experience using the Syncardia Total Artificial Heart in a recent edition of the medical journal Perfusion. See an abstract of the research paper.
Frakes’ team has since performed four other pre-operative planning scenarios with virtual implantations performed by Ryan.
The team has also developed a series of 3-D models of hearts with congenital defects, designed for use in helping physicians plan surgical strategies based on the individual conditions of patients. The venture is called Heart in Your Hand.
The Materialise company recently licensed the entire Heart in Your Hand library of congenital heart defect models and is displaying them on its HeartPrint website.
Heart in Your Hand is also working with St. Joseph’s Medical Center in Phoenix to develop more 3-D congenital heart defect models for educational purposes.
Materialise’s HeartPrint catalogues 3-D models of all types for use in education and clinical trials. “Materialise is the world’s largest 3-D printing service, meaning that Heart in Your Hand models will now be distributed all over the world,” Frakes says.
Says Ryan, “3-D heart models and performance of virtual heart implantations are no longer the inventions of science fiction. They are happening and they are impacting medicine, medical education, and quality of life right now.”
Written by Rosie Gochnour and Joe Kullman
Media Contact:
Joe Kullman, [email protected]
(480) 965-8122
Ira A. Fulton Schools of Engineering