ASU engineer makes mobile health apps more effective

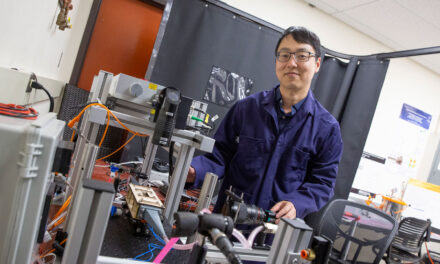
Above: The wealth of real-time health data has enabled Daniel Rivera, a professor of chemical engineering at Arizona State University, to apply control systems engineering techniques to improve mobile health apps. Rivera is collaborating with interdisciplinary teams to develop underlying models and notification systems to deliver effective healthy behavior interventions. Photo: Shutterstock
Looking to make those healthy changes stick? An Ira A. Fulton Schools of Engineering researcher at Arizona State University wants to help.
Plenty of mobile health apps and wearable devices can get you started with increasing healthy behaviors such as walking.
But they often don’t take your unique circumstances into account before sending an alert to remind you to get moving. That leads to alert fatigue — think about how often you find yourself ignoring those nudges from your Apple Watch or Fitbit to stand up or exercise.
That’s where engineers can help tip the scales.
Daniel Rivera, professor of chemical engineering and program director for the Control Systems Engineering Laboratory at ASU, is looking to turn one-size-fits-all mobile health apps into smart digital personal health coaches.
Using the wealth of health data to engineer better apps

Daniel Rivera
Rivera has spent decades applying control systems engineering to various industries, from petrochemical and semiconductor manufacturing processes to addiction and behavioral medicine.
“[Control systems engineering is] all about how systems have variability which may affect important outcomes,” Rivera says. “Control systems engineering is the science that systematically looks at change over time, and how to develop mechanisms that manage variability to optimize these important outcomes.”
In the 2000s, Rivera became interested in how he could apply these skills to get people healthy, whether that’s through fighting addiction or living less sedentary lifestyles.
“The same skill set that is meaningful to chemical engineering problems applies to problems in behavioral medicine,” Rivera says. “It is facilitated by increased access to information and intensive data collection.”
The wealth of data that has come out of mobile health apps and wearables such as Apple Watches and Fitbits makes it possible to apply control systems engineering techniques to behavioral medicine and machine learning to make notifications more helpful and more effective.
“Currently, there is access to data at more frequent intervals than there was in the past, and that offers the opportunity to use the same kinds of methods that would be relevant to a refinery or production plant,” Rivera says.
Multidisciplinary collaboration makes behavioral medicine smarter
Since engineers can’t solve these problems alone, Rivera works alongside researchers from other universities that specialize in behavioral medicine as well as machine learning, data science and human-computer interaction while he contributes his expertise in control systems engineering and experimental design.
“This collaboration is essential,” Rivera says. “We bring a complementary but different set of tools. Everybody needs to be talking to each other because there’s no way that any single discipline can address all these issues. The nature of the problem is more difficult and requires multiple skills to help come up with effective solutions.”
He’s working with his collaborators on a couple of projects recently funded by National Institutes of Health grants to develop dynamic models and just-in-time alerts that maximize the benefits of mobile health apps to increase healthy behaviors over long periods of time.
One of Rivera’s collaborators, Donna Spruijt-Metz, a professor of psychology and preventive medicine at the University of Southern California, praises her research team’s multidisciplinary efforts.
“In the effort to develop new, dynamic models of human behavior that can be used to drive interventions based on ongoing, incoming data in real time, it takes a village,” Spruijt-Metz says. “It takes a close-knit village of disparate researchers from different disciplines who not only see the ‘elephant’ from different angles, but who are willing to translate what they see into shareable languages.”
Spruijt-Metz commends Rivera’s ability to translate complex engineering topics to his collaborators, which enables her team to make strides in solving big challenges in mobile health and behavioral medicine.
“The potential of control systems engineering to understand and change behavior would be totally opaque to the field without Daniel’s willingness to learn to speak our language as behaviorists,” she says. “His ability to take a leap of faith in science, as it were, is what makes him a great thinker.
Rivera is also working with Eric Hekler, a former ASU researcher who is now an associate professor in the Department of Family Medicine and Public Health at the University of California, San Diego, to create more effective just-in-time alerts. An expert in psychology and human-computer interaction, Hekler says the complex behavioral research his team is working on would not be possible without an interdisciplinary team and Rivera’s engineering contributions.
“Daniel was really the inspiration for this [National Institutes of Health grant] proposal as he offered an interesting and novel approach called ‘Model-on-Demand’ to handle the complex issue of notification fatigue,” Hekler says. “There is no way this project would even exist without Daniel.”
Improving the underlying mechanisms of mobile health
In one project, “Operationalizing Behavioral Theory for Mhealth: Dynamics, Context, and Personalization,” funded by the National Cancer Institute, Rivera is working with a research team led by Spruijt-Metz to apply behavioral medicine theories to models and control systems that help make systematic decisions based on data.
“Ultimately, the goal is to obtain useful predictive models that describe behaviors at multiple time scales,” Rivera says.
A thorough stream of data and the right experimental design make it so researchers can learn people’s physical activity preferences across different time intervals, such as within a day or throughout the week.
Some people might prefer to take a walk in the morning, or focus their active time on weekends. Others might prefer to do physical activity when they’re stressed, or are less likely to respond to nudges on a stressful or busy day. Or maybe the weather is bad, so it’s just not a good time for a walk outside.
“A myriad of factors can end up affecting people’s responses to these nudges,” Rivera says. “We’re convinced that control engineering plays a part of it, because ultimately a lot of these variables contribute to changes over time, so a dynamical model can help inform these kinds of decisions.”
Rivera and the research team are specifically adapting social cognitive theory to develop mobile health interventions to increase walking and decrease sedentary behavior. Then, using control systems engineering and machine learning techniques, they are creating verified data-driven models to support mobile health interventions that develop sustained healthy behavior.
This research is part of a focused effort by the NIH to study factors that influence healthy behaviors. Rivera is an investigator for one of seven projects and one coordinating center that form the Intensive Longitudinal Health Behaviors Network.
Anticipating users’ preferences for a personalized approach to mobile health
In a second project funded by the National Library of Medicine, “Control Systems Engineering for Counteracting Notification Fatigue: An Examination of Health Behavior Change,” Rivera is working with Hekler and Predrag Klasnja, assistant professor in the School of Information at the University of Michigan, to develop a novel system of nudges that takes into account a mobile health app user’s personal data to decide when to give nudges and alerts.
If you wear an Apple Watch or Fitbit device, you might get reminders to move or get out of your seat based on set intervals of time.
“What we’re trying to do is, through a structured scientific approach, provide informative notifications that don’t just notify people for the sake of it, but rather notify them at opportune times when they’re most likely to respond and also so participants don’t get annoyed at the notifications or experience notification fatigue,” Rivera says.
Because healthy outcomes are accumulative — the benefits grow as the behavior continues — keeping nudges effective is necessary. And to make them effective, they have to be timed just right. So, fittingly, these alerts are called “just-in-time” notifications.
Similar to the National Cancer Institute funded research, Rivera and the research team are working to estimate dynamical models that will inform decision algorithms as to when to alert users, so nudges and suggestions occur just as they would be receptive to the intervention.
Developing the underlying models to assess when nudges are effective and to deliver them just in time would go a long way toward increasing the effectiveness of mobile health apps.
While it is difficult to precisely predict when this research will make its way to consumer devices, Rivera says the field of mobile health is changing rapidly and estimates that intelligent just-in-time estimation technology may be available commercially within the next five to ten years.
“I have seen great strides in the role of systems and information science for behavioral interventions since my initial interest in the topic in 2003,” Rivera says. “Many enabling technologies are converging to facilitate implementation and make these ideas useful in practice. The question is not ‘if’ but ‘when.’”
In the new decade, these underlying models that assess your preferences paired with just-in-time notifications might be powering your apps to help you achieve your health behavior goals.