A germ of an idea: Turning a virus into a new tool to help brain disorders

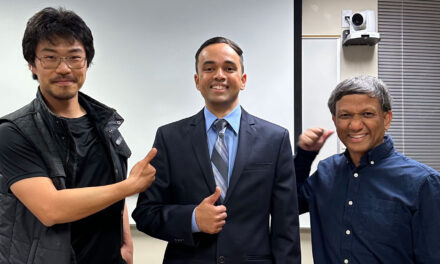
Above: An innovative proposal to engineer the Zika virus into a tool to deliver treatments to the brain for mental illness and neurodegenerative disorders has earned Arizona State University Assistant Professor Benjamin Bartelle an inaugural 1907 Research Trailblazer Award Kissick Fellowship. The two-year grant supports high-risk, but high-impact research that pushes the envelope in the development of new approaches for treating mental illnesses and understand their underlying causes — all leading to better treatment and prevention. Photographer: Connor McKee/ASU
Beneficial molecules are everywhere in nature.
A molecule from the bark of yew trees led to the development of the cancer-fighting drug Paclitaxel. A compound from scorpion venom is being studied as a potential new glioblastoma treatment. These are examples of harvesting bioactivity, and it is not limited to plants and animals.
Benjamin Bartelle, an assistant professor of biomedical engineering in the Ira A. Fulton Schools of Engineering at Arizona State University, is exploring how to harvest bioactivity of the Zika virus to put its natural abilities to good use and help treat mental illness and neurodegeneration.
In its wild form, Zika is an elusive and devastating virus. The mosquito-borne virus caused an outbreak in the Americas in 2015 and was most notably characterized by rashes and microcephaly in newborn babies.
However, Bartelle believes the Zika virus can be engineered into a tool to deliver therapeutic treatments and address inflammation in the brain associated with mental illness, severe depression, schizophrenia and neurodegenerative diseases and disorders — something pharmaceutical companies have been unable to do.
“The field is in crisis and drug companies have given up on neurodegenerative disorders. This is the first step in the larger world of therapies because it has not been done before,” Bartelle says. “We use viruses to carry replacement genes or to carry antigens (substances that promote an immune response) and we even let them infect and kill cells we don’t like. But using the innate biology of a virus as a drug is an entirely new form of therapy.”
The innovative idea of using the Zika virus has earned Bartelle the support of the inaugural 1907 Research Trailblazer Award Kissick Fellowship. This two-year, $120,000 grant supports mental health research proposals with high impact potential by researchers at leading hospitals and universities in the U.S., U.K. and Canada. The Kissick Family Foundation, founded by Kathy and John Kissick and operated by their children Kasey and Ryan, has collaborated with 1907 Research in generously sponsoring this fellowship.
“At 1907 Research, we are focused on neural mechanisms that cause, and can cure, mental illnesses. What attracted us to Dr. Bartelle’s research proposal was the method of delivery — harnessing a virus for modifying cell behaviors,” says Dr. Joshua Rosenblat, co-founder and research director for 1907 Research. “It is uncommon for established foundations to fund this type of research by emerging scientists.”
The importance of addressing mental illness and neurodegenerative diseases
Finding solutions for mental illness has personal significance to Bartelle. While growing up, he struggled with dyslexia and attention deficit disorder, and almost quit school as an undergraduate student due to depression. Bartelle watched as family members and friends were also affected to various degrees by mental illnesses. Many died young as a result of their conditions.
Bartelle is also motivated to combat the tragic way neurodegenerative diseases like Parkinson’s and Alzheimer’s cut lives short or deprive people of their independence and sense of self.
“Mental illness is the most taxing aspect of our society. It gets us at our most dynamic and drags down everything around us,” Bartelle says. “I feel connected to neuroinflammation and neurodegeneration research in a personal way. I’m invested. It’s who I am.”
Bartelle has spent a multifaceted career exploring a variety of solutions to mental illness treatment, including industry and startup efforts in drug development and synthetic biology.
While the work of his neuroimmunity and imaging lab at ASU is interrupted by the COVID-19 pandemic, Bartelle used the time to talk to medical professionals about what was missing in the field. Concluding that drug-based therapies appear to be reaching an impasse in treating neurodegenerative diseases and mental illness, Bartelle started thinking about new ways to manipulate the brain’s immune system. That’s when he came up with the idea to use the Zika virus.
But as a new faculty member proposing a completely new paradigm of mental health and neurodegenerative disease treatment, Bartelle found it difficult to get funding from traditional avenues.
His novel approach, however, fits 1907 Research’s mission to transform the knowledge and outcomes of mental illness through brain and mind research. 1907 Research has developed a blinded grant funding process to make award decisions based on scientific merit and reduce bias.
1907 Research supports unique ideas that would not fall easily within the scope of other more traditional funding organizations, especially proposals involving high-risk, high-reward research pursuits. This public charity seeks to change the future of mental health by supporting the promising early career researchers who could push the envelope to develop new approaches for mental illnesses, understand the underlying causes, and lead to better treatment and prevention of mental illness.
“As a researcher, I have always been a little ‘out there’ and I have not had a lot of luck with independent funding,” Bartelle says. “1907 Research saw the potential for what I was proposing for a wide range of diseases.”
Anil Seth, a professor of cognitive and computational neuroscience at the University of Sussex and member of the 1907 Research Advisory Board that selected the Trailblazer Award Fellows, says this is the type of research he and 1907 Research are looking to support.
“Dr. Bartelle’s research proposal struck me as highly creative and slightly wild — but in a good way,” Seth says. “It feels good to be able to support this kind of high-risk, high-impact research, and especially to back a scientist willing to push boundaries in ways so often neglected by traditional funders.”
The charity received 150 applications from 69 universities and hospitals for the inaugural 1907 Trailblazer Award. Only three Fellows were selected — an acceptance rate of 2%.
The other Trailblazer Award recipients are Laura Lewis from Boston University, who is researching the link between sleep, cerebrospinal fluid flow and inflammation in depression; and Katherine Scangos from the University of California, San Francisco, who is focusing on understanding how disruptions in the interconnected neural networks of the brain contribute to major depression and whether brain stimulation could be a viable therapy.
Understanding neuroimmunity
Our brains have their own immune system. Specialized cells called microglia patrol the brain, looking for possible intruders and harmful substances. They also prune away unused synapses, paving the way for new blood vessels and nerve connections. As part of their duties, microglia cells also regulate inflammation.
Inflammation of nervous tissues, called neuroinflammation, is helpful when it’s used to survive harmful situations such as fighting infections or clearing away damaged tissue. But when the brain is in a state of constant neuroinflammation, microglia stop doing their other important duties, allowing or even driving deteriorating effects to healthy brain tissue.
Microglia dysfunction and neuroinflammation have been strongly linked to brain disorders, such as schizophrenia and neurodegenerative diseases.
It’s unknown exactly what role neuroinflammation plays in conditions like major depressive disorder and schizophrenia, but Bartelle believes it’s worth investigating.
“We know neuroinflammation is at least part of all these things, so it seems like the potential is there,” he says. “We don’t have anything else to go off of in terms of identifying the throughline of these neuropsychiatric disorders.”
Pharmaceutical companies have been unable to design therapies that effectively target microglia or harmful neuroinflammation without leading to further deterioration of brain tissue.
“Despite knowing many of the disease mechanisms that involve neuroimmunity, our capacity to address them therapeutically is severely limited,” Bartelle says. “Most neuroimmune signaling pathways have distinct and even opposite functions in neighboring cell types, rendering microglia incompatible with small molecule approaches. Cell type selective therapies are similarly elusive, as microglia remain intractable even by the most heavily engineered gene therapy vectors.”
The Zika virus, however, is exceptionally good at infecting microglia and often goes undetected. It redirects the cells to suppress inflammation and recycle extra proteins through a process called autophagy — the same processes that become dysregulated in neurodegeneration.
Engineering a potential breakthrough
Scientists and engineers have been able to “domesticate” viruses with careful engineering, but these efforts removed as much bioactivity as possible and focused on how the outer viral surface stimulates the immune system or carries new genes into cells.
Several types of viruses have been domesticated for use in gene therapy and research, including rabies, adeno-associated viruses and HIV. However, none have been used to affect microglia or to address mental illness, neuroimmunity or neurodegenerative diseases in this way.
Bartelle is taking a different approach with the Zika virus by keeping much of its genome intact, harnessing Zika’s positive bioactivities and suppressing its negative traits through a process called continuous directed evolution.
His method causes mutations in Zika virus while creating selection criteria for things they do or don’t want the virus to do. The method selects for positive traits, such as ones that will help deliver treatments to microglia, for enhanced survival for the next generation. Negative traits, like an antiviral response, are keyed to a gene circuit that activates a “suicide gene,” blocking viral replication. Through this process, the Zika virus can be selectively bred to transform it into something beneficial.
It’s a complex process, and not something scientists often do because results can be unpredictable. However, Bartelle has years of experience bringing technologies from the drawing board to their application. He believes new advances have allowed this complexity to become a strength that can be harnessed to engineer more robust systems. He has partnered with other researchers and implemented methods in synthetic biology, human microglia animal models, and viral assisted and continuous evolution methods of bioengineering to create this new virus-based delivery tool.
“We have every element in place for harnessing the microglia-specific capacity of the Zika virus to suppress inflammation and stimulate autophagy into therapies with a potential beyond anything available,” Bartelle says.
With the support from 1907 Research, Bartelle will use directed evolution to engineer the Zika virus to “infect” microglia cells and deliver gene therapies that will help microglia successfully regulate inflammation and carry out their duties.
Guoping Feng, a professor of neuroscience at Massachusetts Institute of Technology who serves on the 1907 Research Advisory Board that selected the Trailblazer Award Fellows, says Bartelle’s idea to take advantage of the natural ability of the Zika virus to invade microglia and tweak it to make it a safe tool for research is a creative one.
“Dr. Bartelle proposes to develop a viral vector that would allow scientists to deliver different molecular tools into microglial cells,” Feng says. “If successful, this will be a transformative tool for the field and dramatically accelerate the research on microglia. His research could have broad impact beyond mental illness because microglia dysfunction has also been strongly linked to neurodegenerative disorders.”
A new paradigm of treatments
“Coming in with an open mind has led to more success than approaching something with the assumption it will work,” Bartelle says. “So, I’m not worried about this project failing. As long as we keep a flexible approach, something will come out of it.”
Bartelle says he hopes to get to clinical trials within five years to treat severe, life-threatening forms of neurodegenerative diseases by using these domesticated virus particles to carry treatments to microglia cells. If the method can be validated with severe neurodegenerative diseases, it could then be expanded for use in mental illness like schizophrenia or severe depression.
He also hopes to help create a new community of biological device researchers who can investigate new areas of research in the School of Biological and Health Systems Engineering, one of the six Fulton Schools, and beyond.
“You can contribute something new that has value,” he says, “but it’s not until you have cooperation with a large community that you can make progress.”
Once the infrastructure is in place to direct the evolution and domestication of the Zika virus — which Bartelle hopes to achieve within a few years — it can be used for a wide variety of outputs. For example, the dengue virus affects the liver, and inflammation from fatty liver disease is a rising cause of death in the U.S. So, researchers can adapt the same process Bartelle hopes to develop for the Zika virus to support a new class of therapies for liver diseases with domesticated dengue virus.
“For each element in the chain of pathologies,” Bartelle says, “we can build new viruses that go after these things, and create a pipeline for a whole new class of therapies.”